Let’s Prevent TB-IRIS in Patients with HIV: An Important Guidelines Update for Your Clinical Practice
By:
- Alaa Makawi, PharmD Candidate
College of Pharmacy, Nova Southeastern University - Dayamie Othello, PharmD Candidate
College of Pharmacy, Nova Southeastern University - Elizabeth Sherman, PharmD, AAHIVP
College of Pharmacy, Nova Southeastern University
South Florida, Southeast AIDS Education and Training Center
Tuberculosis-immune reconstitution inflammatory syndrome (TB-IRIS) is an early complication associated with the initiation of antiretroviral therapy (ART) in patients co-infected with TB and human immunodeficiency virus (HIV). Earlier initiation of ART in patients co-infected with TB reduces mortality among patients with low CD4 counts; however, it increases the risk of paradoxical TB-IRIS.1 Opportunistic infection guidelines offer updated recommendations on when to start ART in persons with co-infection after initiating TB treatment. ART should be initiated within 2 weeks in patients who have a CD4+ count <50 cells/mm3. Importantly, ART should be started within 8 weeks in patients who have a CD4+ count > 50 cells/mm3 (an update from previous guidelines recommending starting ART within 8-12 weeks). TB-IRIS is thought to occur as a result of a recovering immune system after starting ART which drives inflammatory reactions directed at the mycobacterium TB antigen, the bacteria that causes TB disease.1
Paradoxical TB-IRIS occurs in individuals who have already been diagnosed with TB prior to starting ART. Within 1 to 4 weeks of ART initiation, patients begin to develop new or recurrent symptoms as well as new worsening or recurrent clinical and radiologic features of TB.1 Patients who are at greater risk for developing paradoxical TB-IRIS include those with CD4+ count less than <100 cells/mm3, high HIV viral load prior to starting ART, disseminated TB, and a short interval between starting TB treatment and initiating ART.1 A recent study explored pre-emptive prednisone treatment for prevention of paradoxical TB-IRIS and based on the study results, the opportunistic infection guidelines offer new recommendations. It is important for prescribers to be aware of these updated recommendations and incorporate these changes into their clinical practice.
This recommendation is based on the prednisone for the prevention of paradoxical TB-associated IRIS trial. The trial was a randomized, double-blind, placebo-controlled trial performed at a a government-run outpatient primary care HIV–TB clinic in South Africa (). 240 high-risk patients were enrolled who met the following inclusion criteria: diagnosed with HIV who had not previously received ART and now initiating ART, CD4 count of ≤100 cells /mm3, microbiologically confirmed TB or a clinical diagnosis with symptomatic response to anti-TB treatment, and receiving anti-TB treatment for less than 30 days before initiating ART.2 Exclusion criteria were Kaposi’s sarcoma, pregnancy, neurologic or pericardial tuberculosis, rifampin-resistant tuberculosis, hepatitis B infection, receipt of nonstandard antituberculosis treatment, poor clinical response to antituberculosis treatment before the start of ART, uncontrolled diabetes, an alanine aminotransferase level of more than 200 IU per liter, an absolute neutrophil count of less than 500 mm3, and systemic glucocorticoid use within the previous 7 days2. Randomization was performed in a 1:1 ratio and patients were randomized into two groups, the prednisone group and the placebo group.2 Patients in the prednisone group received 40 mg of oral prednisone per day for 14 days, followed by 20 mg per day for 14 days.2 The prednisone or placebo was started within 48 hours after the initiation of ART2.The outcome of the trial showed the incidence of TB-IRIS was 30% lower in prednisone group than in placebo group (relative risk, 0.70 (95% CI, 0.51–0.96) P=0.03). 2 Based on these study findings, the opportunistic infection guidelines now recommend that pre-emptive prednisone therapy should be offered to prevent TB-IRIS in high-risk patients with a CD4 count ≤100/mm3 who are starting ART in the context of recently initiated anti-TB therapy, are responding well to TB therapy, and who do not have rifampin resistance, Kaposi’s sarcoma, or active hepatitis B2.
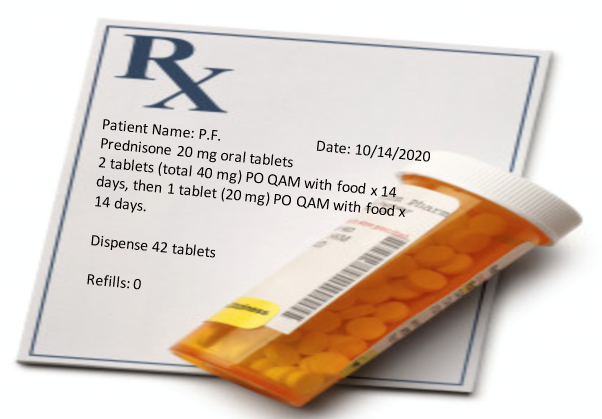
In summary paradoxical TB-IRIS occurs at a higher rate in those co-infected with HIV and a low CD4+ count. Pre-emptive prednisone should be offered to persons at high risk for developing paradoxical TB-IRIS. Prescribers should initiate prednisone oral tablets 40 mg per day for two weeks followed by 20 mg per day for two weeks (see figure 1). Clinicians should be aware of this important update to the opportunistic infection guidelines and incorporate these changes into their clinical practice.
Figure 1. Sample prescription for pre-emptive prednisone for the prevention of paradoxical TB-IRIS.
References:
- Panel on Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV. Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-infected Adults and Adolescents: Recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIVMedicine Association of the Infectious Diseases Society of America. Available at https://clinicalinfo.hiv.gov/sites/default/files/inline-files/adult_oi.pdf. Accessed 10 Oct. 2020
- Meintjes G, Stek C, Blumenthal L, et al. Prednisone for the Prevention of Paradoxical Tuberculosis-Associated IRIS. N Engl J Med. 2018;379(20):1915-1925. doi:10.1056/NEJMoa1800762